RPS Training Courses (Who attends?) – Part 4 – Medical
Published: Mar 15, 2019
[Update September 2023 - these blog posts are a few years old now, but still provide useful content regarding the types of delegates we have on our RPS training courses. If you work in the medical sector then please read on, and then consider our online RPS training course. There is no doubt that the C-19 pandemic changed much, but we are delighted that during that time and right now in 2023, medical delegates from the NHS and private sector are still taking our flagship online RPS course. We have pointed out endlessly that it is NOT a course designed specifically for the medical sector, but does contain lots of medical content (since this is interesting for all delegates). Many of our medical related delegates have commented that they appreciated understanding the bigger picture of radiation protection outside their own particular work areas.
Also note as of October 2023, we are very close to releasing our Radiation Safety Awareness: Uses of ionising radiation in the medical sector course. This awareness course covers specialist staff who work directly with ionising radiation, non-specialist staff working in departments where ionising radiation may be present, and other staff who may have contact with patients who have been administered with radioactive material (e.g. PET)].
Ionactive Radiation Protection Supervisor (RPS) training courses are designed for all users of ionising radiation, and it is pleasing to see so many medical related delegates attend. It may interest the reader to know that Ionactive is Radiation Protection Adviser to some of the biggest companies in this sector (including GE Healthcare, Philips Medical Systems, and Elekta Oncology Limited). We have delivered bespoke training to these companies (and others), however the subject of this blog post is attendees on our two-day RPS training course.
When medical related delegates apply for a place, we make it clear that the course is not medical biased, it is designed for all uses of ionising radiation from all sectors. That said, we also make clear to all delegates (during our introductory sessions on Day 1) that medical exposures are always considered and discussed as they are a significant comparator to use when discussing radiation risk. We have always believed that mixing up delegates from all areas of ionising radiation use produces a better RPS – the delegate learns to understand the radiation risks in their area, in context with other sectors. This is particularly true of the medical delegate since they are deliberately exposing patients to ionising radiation (under strictly controlled conditions), whilst keeping their own exposures (including colleagues and members of the public) to ALARP levels (as low as reasonably practicable) and always below dose limits. The whole group (medical and non-medical) gain a good appreciation of the concept of benefit outweighing radiation risk (where the pivot point differs between medical and occupational exposure).
We also make clear that IRMER (Ionising Radiation (Medical Exposure) Regulations 2017) are not a significant consideration in the course (although our legislation course notes consider IRMER in some detail). This is a useful and important distinction since the Ionising Radiations Regulations 2017 (IRR17) deal with occupational exposure, whereas IRMER deals with patient exposure. (It is true that critical examinations under IRR17 for medical equipment do also consider patient exposures). Local rules (which are supervised by the RPS) are defined in IRR17 and not IRMER. Whilst we have seen IRMER considerations in Local Rules, we believe they should be treated completely separately. A medical delegate attending one of our RPS courses will receive all they need with respect to IRR17, with only minimal consideration of IRMER (this should be the subject of a separate training course). As mentioned at the beginning, this approach works as we see many delegates from medicine, including repeat attendees.
Delegates come from industry supporting the medical sector (e.g. F-18 production, cyclotron engineering, medical equipment suppliers), and directly from hospitals and clinics where patients are treated. In the following sections, we summarise some of these.
F-18 Production
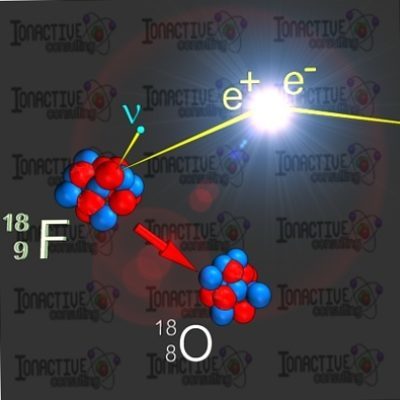
F-18 is a radioactive positron emitter which is used in the diagnostic procedure PET (positron emission tomography). PET is an imaging technique where F-18 is attached to a glucose carrier which is taken up by the body (via injection, the mouth etc). The resulting annihilation radiation (produced via a positron-electron interaction) is picked up by sensitive detectors which can then provide important metabolic data and clinical diagnosis. Since F-18 has a very short half-life (110 minutes) it has to be made very close to the patient (i.e. at the hospital or at local centers). F-18 is produced in a cyclotron which is run in the early hours of the morning (this ensures a build-up of desired radioactivity since F-18 is decaying away as its produced). Technicians then remove the F-18 from the cyclotron target in special shielded cells where further radio-pharmaceutical procedures are undertaken (i.e. radio-labelling, quality assurance checks etc).
The radioactivity of a ‘patient dose’ (nominally 400 MBq) is far higher at the point of manufacture since account must be taken of the decay time between the shielded Fludeoxyglucose leaving production, to the point where it can be delivered to the patient in a nuclear medicine department. RPS delegates from commercial companies or hospitals which produce F-18 are regular attendees on Ionactive courses. Delegates may be involved with the operation and in-house service of the cyclotron, the radiopharmacy production cells, quality assurance, and transport. The potential dose rates from working in these areas are not trivial. When the cyclotron is shut down for maintenance/service etc parts of it remain active ‘hot’ – due to neutron activation of components. This situation improves with time and depends on the individual half-life of the radioactive material produced via activation. Working with F-18 can also yield high dose rates to the trunk of the body or extremities (e.g. finger doses when undertaking quality control procedures with stock vials). Furthermore, F-18(FDG) is readily taken up by the body (which is the point for patient diagnostics, but undesirable for occupational exposure control). Therefore, careful attention must be given to avoiding inhalation of ingestion of the F-18. These are all important considerations for an RPS who works in this area.
Medical equipment (manufacturer, supplier, and installer)
As noted earlier, Ionactive provides RPA services for a number of medical related companies. Therefore, it is not unusual for us to provide bespoke in-house RPS training for their employees including equipment designers, sales staff, modality training and installation/service engineers. However, we still see many delegates representing diagnostic imaging, radiotherapy, and brachytherapy. Since the equipment/technique is the same regardless of job function, we will consider individual modalities in the sections which follow.
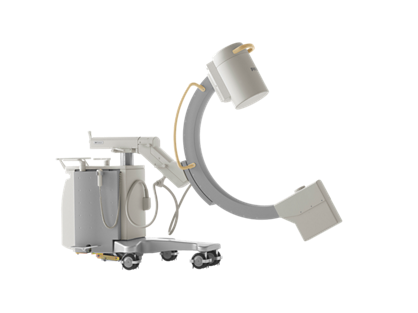
Hospital - Diagnostics
Diagnostic radiology in hospitals and clinics covers a wide area of ionising radiation use. Equipment ranges from simple conventional x-ray (we often use the word ‘flash x-ray’ since they take a picture with a short mS exposure time), to more exotic systems including real-time x-ray fluoroscopy producing moving images and CT (computed tomography) producing 3d images that can be manipulated in real time. For the RPS there are many considerations such as the use of mobile x-ray (where the controlled area is defined by ‘sight’) to ensuring inadvertent unintended exposures are avoided. Following the local rules is a given, but in a busy work environment with patients, vigilance is equally important. It is quite possible that x-ray fluoroscopy could be used in a life-saving event (positioning a stent to unblock clogged heart arteries) – during this time the patient is receiving obvious net benefit, whereas the person carrying out the procedure needs to be aware of exposures to their hands (avoid placing hands directly in the x-ray beam) and their eyes (are they wearing eye protection?). The RPS (who may be a nurse in attendance) needs to be aware of the use of dosimetry (or lack of), and the wearing of personal protective equipment (PPE) such as leaded aprons.
Hospital - Radiotherapy

One of the advantages of having delegates from the radiotherapy sector on our RPS training courses is the way they nod knowingly when we begin to talk about deterministic effects from very high doses of radiation (certainly >> 1 Gy delivered over a short period of time). Traditionally most radiation safety courses look at the negatives of such exposures (and there are plenty with respect to occupational exposures!), without spending a little time considering if there are any benefits. Mark Ramsay of Ionactive has spent many a time in training courses in an earlier life where pictures of radiation burns were presented as a warning (‘radiation is evil stuff’), without any consideration of the good that such high radiation doses can yield. So in our training courses, the odd radiation burn might be shown (we warn you, so you can look away…), but at the same time, a picture of Mrs. Ramsay is proudly displayed post breast cancer radiotherapy (she is fine now 😊 ).
The most common type of radiotherapy system is the linear accelerator (linac) and these are generally located in concrete shielded bunkers with a maze to allow patient/staff access. Less often the maze is replaced with a large shielding door (usually to save space). The linac operates in the energy range of 6-25 MV photons (with 10 MV probably being the most common). Direct electron beam treatment is also available. The safety systems for such treatment rooms are comprehensive (both for patient and staff). Active and passive safety signage, interlocked doors, light curtains, last person out buttons, audible alarms, interlock confirm buttons, emergency stops, treatment interrupts etc. These are all specified in the radiation local rules and the RPS is responsible for ensuring that the rules are strictly followed. For example, the ‘last person out’ button starts the safety interlock sequence once the patient has been made ready for treatment, and it really does mean ‘last person’ (not whoever is near it at the time of leaving the treatment room).
Hospital - Brachytherapy
Despite modern brachytherapy systems being technically advanced (from both safety and patient treatment perspectives), the actual technique is older than external beam radiotherapy (as noted above). It is true that before linac external beam therapy was popular, Co-60 teletherapy systems were employed. However, the internal treatment of cancers with brachytherapy can be dated back to the first uses of Ra-226 (radium). Brachytherapy places a source of ionising radiation (i.e. a sealed radioactive source) directly into the area being treated. Such techniques are useful for prostate, bladder and cervical cancer etc. In the early days (and this is still applicable today for certain techniques), the sealed source is in the form of a ‘seed’ which is manually placed into the treatment area. Permanent seed brachytherapy (low dose-rate brachytherapy) may use I-125 seeds (half-life 60 days) and these are left in the patient until they decay to negligible levels of radioactivity. Modern techniques using sophisticated after-loader systems (often delivering high dose brachytherapy) employ Ir-192 sources of high activity (typically 470 GBq). An Ir-192 source of this activity, exposed directly in air unshielded, would deliver a dose rate of 53mSv/h at 1m. Therefore, these systems deliver the source to the patient (and remove it after the set treatment time) using an automated system in a shielded room. This area has safety features not dissimilar to those described for the linac treatment areas in the proceeding section.
A big difference when compared to the linac, is that the linac can be switched off, whereas the Ir-192 sources can only be shielded. Therefore, the RPS for this type of facility has to be particularly aware of the contingency arrangements - for example dealing with a radioactive source that fails to return to the shielded container post-treatment. In addition, the RPS needs to ensure that local rules are suitable for source wipe tests (generally undertaken by service engineer), source exchanges (Ir-192 has a relatively short half-life of 74 days) and all the security aspects dealing with High Activity Sealed Sources (HASS).

Other medical related ionising radiation sources
We will conclude this latest blog post by a quick mention of some less common but fascinating medical treatment systems. We have RPS training delegates working with all the systems mentioned in this section. In addition, Ionactive is fortunate to be involved in providing Radiation Protection Adviser services and undertaking shielding design calculations across a broad range of these.
The Gamma Knife is a stereotactic radiosurgery system for the treatment of brain tumors (and other nerve-related symptoms such as facial pain). The system uses 192, 1TBq Co-60 radioactive sources arranged into a heavily shielded source holder with selective collimators. Like brachytherapy mentioned above, the RPS in this area will be concerned with radiation safety and security (since each of the 192 sources has HASS status).
Ionactive has been involved in the early development of the Elekta Unity ‘MRI Radiotherapy’ system (including shielding design and safety system endorsements for R&D bunkers) and more recently in the shielding design of clinical installations of Unity at hospital sites.
If you work in this sector and need RPS training, then how about checking out our online RPS training course. If you prefer face to face training then please consider asking colleagues to organise an in-house Ionactive RPS training course - we would be happy to deliver this at your place of work.
Mark Ramsay is a Radiation Protection Adviser (RPA) and Radioactive Waste adviser (RWA) with Ionactive Consulting Limited.
